Navigating Pharmaceutical Deviations: Your Essential Management Checklist
Published: 11/25/2025 Updated: 12/14/2025
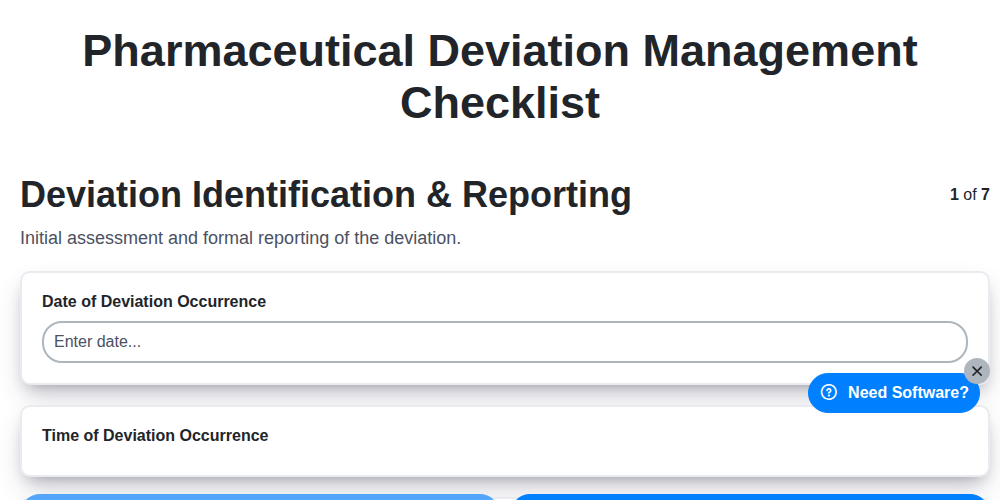
Table of Contents
- Understanding Pharmaceutical Deviation Management
- Deviation Identification & Reporting: The First Step
- Thorough Deviation Investigation: Root Cause Analysis
- Corrective and Preventive Actions (CAPA): Planning for Improvement
- CAPA Effectiveness Verification: Ensuring Lasting Impact
- Documentation & Record Keeping: Maintaining a Clear Audit Trail
- Risk Assessment & Impact Analysis: Identifying Potential Risks
- Closure & Review: Formalizing the Process
- Continuous Improvement: Beyond the Checklist
- Resources & Links
TLDR: Pharmaceutical deviations happen. This checklist template breaks down the entire process - from spotting & reporting them to fixing the root cause (CAPA), verifying it worked, and documenting everything - into manageable steps. Use it to ensure compliance, minimize risk, and streamline your deviation management process.
Understanding Pharmaceutical Deviation Management
In the highly regulated pharmaceutical industry, maintaining product quality, patient safety, and regulatory compliance is paramount. A crucial element of this is robust deviation management. A deviation, simply put, is any unplanned event or observation that departs from established procedures, specifications, or processes. These can range from minor discrepancies to significant errors impacting product quality.
Deviation management isn't about assigning blame; it's about proactively identifying vulnerabilities in your system, understanding why deviations occur, and implementing changes to prevent recurrence. Effective deviation management demonstrates a commitment to continuous improvement and provides a vital line of defense against potential quality failures. It's a structured process involving multiple steps, each designed to thoroughly investigate the event, determine root causes, and implement preventative measures. Failing to adequately manage deviations can result in regulatory sanctions, product recalls, and, most importantly, harm to patients. This article will explore the key components of a comprehensive pharmaceutical deviation management checklist, ensuring your process is thorough and compliant.
Deviation Identification & Reporting: The First Step
The foundation of any robust pharmaceutical deviation management system lies in accurate and timely identification and reporting. This initial step isn't just about flagging an anomaly; it's about establishing a clear, accessible, and non-punitive process that encourages personnel at all levels to recognize and report deviations promptly.
What constitutes a deviation? A deviation is any departure from approved procedures, specifications, instructions, or regulations. This can encompass a wide range of events - from minor discrepancies in manufacturing processes to significant errors in data entry.
Key Considerations for Effective Identification & Reporting:
- Training: Provide comprehensive training to all personnel on what constitutes a deviation, how to recognize them, and the importance of reporting.
- Clear Reporting Channels: Establish multiple accessible reporting channels (e.g., electronic forms, designated personnel, anonymous reporting options) to ensure ease of reporting.
- Non-Punitive Culture: Foster a culture where employees feel safe to report deviations without fear of blame. Transparency and a focus on learning from mistakes are crucial.
- Defined Thresholds: Clearly define reporting thresholds - what needs to be formally documented versus what can be addressed through routine corrections.
- Initial Assessment: Upon receipt of a reported deviation, conduct a preliminary assessment to determine its severity and potential impact. This helps prioritize investigations.
Effective identification and reporting aren't merely about checking boxes; they's about building a proactive safety net for your pharmaceutical processes.
Thorough Deviation Investigation: Root Cause Analysis
A robust deviation management system hinges on a meticulous investigation process. Simply identifying a deviation and noting it isn't enough; understanding why it occurred is paramount. This requires moving beyond superficial observations and delving into a thorough root cause analysis.
The investigation shouldn't stop at the immediate cause - the action that directly triggered the deviation. Instead, it should explore the underlying factors that allowed that action to happen. Employ tools like the 5 Whys technique - repeatedly asking Why? to peel back layers of contributing factors. Consider using a fishbone (Ishikawa) diagram to visually map out potential causes across categories like people, process, equipment, materials, and environment.
During the investigation, gather comprehensive data. This includes interviewing involved personnel, reviewing batch records, equipment logs, training records, and relevant procedures. Don't shy away from uncomfortable truths; objective assessment is crucial for identifying systemic issues. Consider whether the deviation is indicative of a broader training gap, procedural deficiency, or equipment malfunction. Assign clear responsibilities for data gathering and analysis, and ensure the investigation team possesses the necessary expertise to evaluate the findings. The investigation report should be detailed, factual, and include all supporting documentation.
Corrective and Preventive Actions (CAPA): Planning for Improvement
The investigation phase identifies the root cause of the deviation - but that's only half the battle. The true value of deviation management lies in the implementation of effective Corrective and Preventive Actions (CAPA). This section focuses on not just fixing the immediate problem, but preventing it from happening again, and proactively addressing potential future issues.
Planning & Prioritization:
Before diving into action, clearly define the scope of the CAPA plan. What specific actions will be taken? Who is responsible for each action? Set realistic timelines and milestones. Prioritize CAPAs based on the severity of the deviation and the potential impact on product quality and patient safety. High-risk deviations warrant immediate and comprehensive action.
Developing Actionable CAPAs:
CAPAs should be specific, measurable, achievable, relevant, and time-bound (SMART). For corrective actions, these directly address the identified root cause. Preventive actions, on the other hand, are proactive steps taken to eliminate or mitigate potential issues before they occur. Consider:
- Training: Were personnel adequately trained? If not, implement revised training programs.
- Procedure Updates: Were procedures unclear or inadequate? Revise and clarify documented procedures.
- Equipment Maintenance: Was equipment failure a contributing factor? Implement or strengthen preventative maintenance schedules.
- Design Changes: Are process or product design elements contributing to the deviation? Explore design changes to eliminate the cause.
- System Improvements: Are there systemic issues impacting the process? Consider broader system improvements to address the root cause.
Documentation is Key:
Meticulously document all planned CAPAs, including responsibilities, timelines, and expected outcomes. Track progress against the plan and adjust as needed. This documentation is crucial for demonstrating CAPA effectiveness and providing an audit trail.
CAPA Effectiveness Verification: Ensuring Lasting Impact
Implementing Corrective and Preventive Actions (CAPAs) is only half the battle. Truly effective deviation management requires rigorous verification to ensure those actions are actually resolving the root cause and preventing recurrence. This phase isn't simply a formality; it's a critical step in demonstrating continuous improvement and maintaining compliance.
CAPA effectiveness verification involves a defined timeframe and specific methods to assess whether the implemented CAPA achieved its intended results. This goes beyond just checking that the actions were done; it evaluates if the problem is truly solved.
Here's what effective verification should encompass:
- Defined Metrics: Establish objective, measurable metrics before CAPA implementation. These could include reduced deviation frequency, improved process performance, decreased error rates, or improved training outcomes.
- Data Collection & Analysis: Collect data relevant to your established metrics during the verification period. Analyze this data to determine if there's a demonstrable improvement. Statistical process control (SPC) charts can be invaluable here.
- Trend Monitoring: Don't just look at a snapshot in time. Monitor trends to ensure the improvement is sustained over a longer period.
- Auditing & Observation: Conduct audits and direct observations to assess adherence to the CAPA and identify any unforeseen consequences.
- Stakeholder Feedback: Gather input from relevant personnel involved in the process. Their practical experience can highlight subtle impacts that data might miss.
- Documentation: Thoroughly document the verification activities, findings, and conclusions. This demonstrates due diligence and supports your quality system.
If the verification reveals the CAPA is ineffective, the process needs to be revisited. This might involve further investigation, adjustments to the CAPA, or even a complete redesign of the action plan. CAPA effectiveness verification isn't about finding fault; it's about proactively ensuring your quality system is robust and continuously improving.
Documentation & Record Keeping: Maintaining a Clear Audit Trail
Robust documentation and meticulous record-keeping are the bedrock of any effective pharmaceutical deviation management system. It's not simply about ticking boxes; it's about creating a comprehensive, auditable trail that demonstrates a commitment to quality and patient safety.
This section focuses on ensuring that everything related to a deviation is thoroughly documented. This includes, but isn't limited to:
- Initial Reporting: Document the person who identified the deviation, the date and time of the observation, and a preliminary description of the event. Use standardized reporting forms.
- Investigation Records: Detailed notes from investigation team meetings - attendees, discussions, data reviewed, analyses performed, and conclusions drawn. Don't omit negative findings; they are valuable learning opportunities.
- CAPA Plans: Clearly outline the proposed corrective and preventive actions, including specific tasks, responsible individuals, timelines, and expected outcomes.
- Verification Data: Record all data used to verify the effectiveness of implemented CAPAs. Include raw data, analysis, and conclusions.
- Risk Assessment Results: Document the rationale behind the risk assessment, including identified hazards, severity, probability, and resulting risk levels.
- Review Outcomes: Record findings from deviation management reviews, highlighting trends, recurring issues, and areas for improvement in the system.
Key Considerations:
- Good Documentation Practices (GDP): Adhere strictly to GDP principles, including legibility, accuracy, contemporaneousness, and original records retention.
- Electronic Systems: If using electronic systems, ensure they are validated, secure, and provide audit trails.
- Version Control: Implement rigorous version control for all documents related to deviation management.
- Retention Policies: Establish and maintain a defined record retention policy that complies with regulatory requirements.
Insufficient or incomplete documentation can seriously undermine the credibility of your deviation management system, making it vulnerable to regulatory scrutiny. A clear, comprehensive audit trail demonstrates a proactive approach to quality and a commitment to continuous improvement.
Risk Assessment & Impact Analysis: Identifying Potential Risks
Deviation management isn't just about fixing what's already gone wrong; it's about preventing future occurrences. A robust risk assessment and impact analysis are vital components of a proactive pharmaceutical deviation management system. This stage goes beyond simply understanding what happened to evaluate why it happened and what the potential consequences are.
Here's why this step is crucial:
- Prioritization: Not all deviations are created equal. Risk assessment helps prioritize investigations based on potential impact, ensuring resources are focused where they're most needed. A deviation with a high probability of impacting patient safety or product quality demands immediate and intensive attention.
- Root Cause Identification: Understanding the potential impact can often illuminate potential root causes. For example, if a deviation could potentially affect batch release, it forces deeper probing into system controls and procedures.
- Impact Scope: Determine the scope of the impact. Did the deviation only affect a single batch, or could it have wider implications for equipment, processes, or even other products? Consider potential impact on:
- Product Quality: Impurities, potency, stability.
- Patient Safety: Direct impact on patient health or potential for adverse events.
- Regulatory Compliance: Potential for warning letters, recalls, or other enforcement actions.
- Reputation: Damage to the company's image and brand trust.
- Tools and Techniques: Common risk assessment methodologies include Failure Mode and Effects Analysis (FMEA), Hazard Analysis and Critical Control Points (HACCP) principles, and simple risk matrices (probability vs. severity).
By thoroughly assessing the risks and potential impact of each deviation, you move beyond reactive problem-solving and establish a framework for continuous improvement and enhanced patient safety.
Closure & Review: Formalizing the Process
The final, crucial step in deviation management isn't simply about resolving the issue; it's about formally closing the deviation and reviewing the entire process to ensure continuous improvement. This involves a structured closure process and a critical retrospective analysis.
Closure Activities:
- Verification of CAPA Completion: Ensure all actions outlined in the CAPA plan have been fully implemented and documented. This includes confirming that any training, process changes, or equipment modifications have been finalized.
- Sign-off & Approval: A designated, authorized individual (typically with management responsibility) should formally sign off on the deviation closure, signifying their review and acceptance of the corrective and preventive actions. This demonstrates accountability and confirms that the deviation is considered resolved.
- Deviation Status Update: Officially close the deviation within the deviation management system, marking it as "Closed" or similar terminology based on your organization's procedures.
- Notification & Communication: Inform relevant stakeholders (e.g., quality assurance, production, affected departments) that the deviation has been closed.
Review and Learning:
Beyond closure, a thorough review is essential. This should encompass:
- Root Cause Analysis Effectiveness: Was the initial root cause analysis accurate? Did the CAPA effectively address the identified root cause?
- Systemic Issues Identification: Did the deviation highlight any underlying systemic issues within processes, procedures, or training?
- Process Improvement Opportunities: Are there opportunities to improve the deviation management process itself-perhaps streamlining reporting, investigation, or CAPA implementation?
- Trend Analysis: Incorporate the deviation data into trend analysis to identify potential recurring issues and proactively prevent future occurrences.
The closure & review phase isn't just a formality; it's a cornerstone of a robust pharmaceutical quality system, driving continuous improvement and strengthening overall product quality and patient safety.
Continuous Improvement: Beyond the Checklist
While a pharmaceutical deviation management checklist provides a crucial framework, truly excelling in this area goes beyond simply ticking boxes. Consider the checklist as a baseline - a foundation upon which to build a culture of continuous improvement. Regularly review the checklist itself. Are the steps still comprehensive? Do they reflect evolving regulatory guidelines or advancements in technology? Encourage open communication and feedback from all involved, not just to report deviations, but to suggest improvements to the processes that prevent them. Think about root cause analysis training for investigators, explore digital solutions to streamline documentation and analysis, and most importantly, foster an environment where identifying and addressing process weaknesses is seen as an opportunity for growth, not a cause for blame. This proactive approach, focusing on systemic improvements and learning from every deviation, elevates your pharmaceutical deviation management from a reactive exercise to a powerful engine for enhanced product quality and patient safety.
Resources & Links
- U.S. Food and Drug Administration (FDA): The FDA is the primary regulatory body for pharmaceuticals in the U.S. Their website contains guidance documents, regulations, and information related to quality systems, including deviation management. Look for GMP (Good Manufacturing Practice) guidelines and inspection reports.
- European Medicines Agency (EMA): The EMA regulates medicines in Europe. Their website offers guidelines and documents related to GMP, pharmacovigilance, and quality management systems relevant to deviation management. Especially useful for global compliance perspectives.
- International Society for Pharmaceutical Engineering (ISPE): ISPE provides resources, publications, and training on pharmaceutical manufacturing and quality. They often have guidance documents and webinars covering quality systems and deviation management best practices. Membership may be required for some resources.
- Pharmaceutical Online: A comprehensive online resource for pharmaceutical professionals. Search their site for articles and webinars related to quality, regulatory compliance, and deviation management. Provides current industry perspectives.
- Quality Assurance World: Dedicated to quality professionals across industries, including pharmaceuticals. Offers articles, webinars, and resources on quality systems, audits, and continuous improvement, all relevant to deviation management.
- American Society for Quality (ASQ): ASQ is a global leader in quality. Their website provides information, training, and resources on quality principles, tools, and methodologies, many applicable to pharmaceutical deviation management (e.g., root cause analysis, CAPA, statistical process control).
- PwC - Pharmaceutical & Life Sciences: PwC provides consulting services and insights for the pharmaceutical industry. Their website often publishes reports and articles on regulatory compliance, risk management, and quality systems which can inform a robust deviation management program.
- Deloitte - Life Sciences: Similar to PwC, Deloitte provides consulting and industry insights. Look for publications related to quality management and regulatory compliance within the pharmaceutical sector. Offers a macro perspective on industry trends.
- Compliance World: This resource delivers comprehensive regulatory and compliance solutions. Articles and resources cover quality management, deviation investigations, and CAPA processes, crucial for a compliant pharmaceutical operation.
- GMP Compliance: Provides news, articles, and training on GMP compliance. Good resource for understanding current regulatory expectations and common deviation pitfalls within pharmaceutical manufacturing. Covers a variety of topical GMP subjects.
FAQ
What are some common red flags that indicate our deviation management system needs improvement?
Red flags include increasing frequency of deviations, recurring deviations, CAPAs that are ineffective, lack of root cause identification, inadequate documentation, and lack of senior management oversight.
Found this Article helpful?
Pharmaceutical Management Solution
Navigating complex regulations and ensuring quality in pharmaceutical manufacturing? ChecklistGuro's Work OS platform streamlines processes from R&D to production, packaging, and distribution. Maintain compliance, improve efficiency, and reduce risk. Discover how ChecklistGuro can transform your pharmaceutical operations!
Related Articles
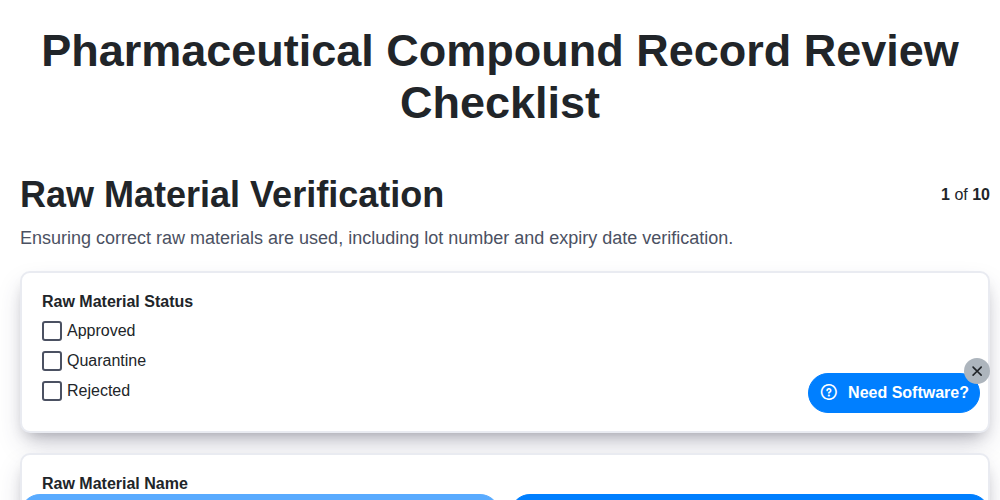
Ensuring Quality: A Pharmaceutical Compound Record Review Checklist Guide
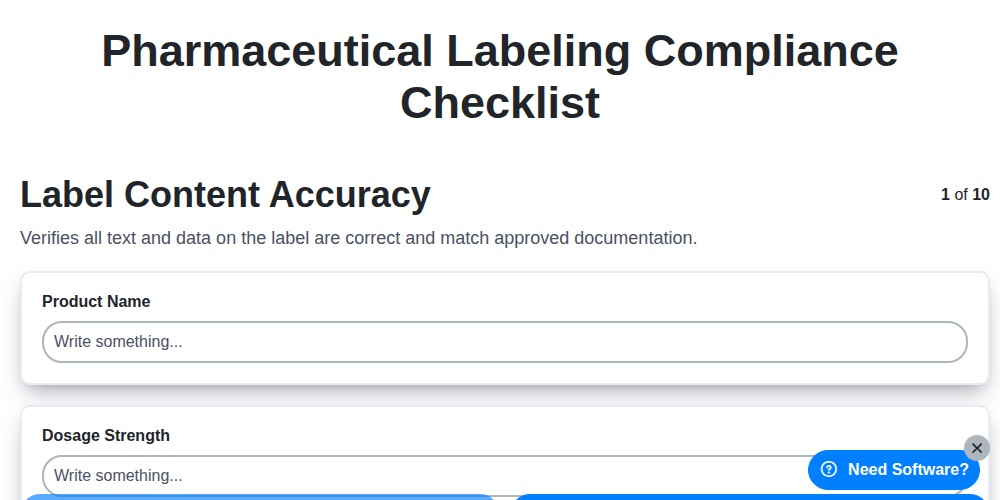
Pharmaceutical Labeling Compliance Checklist: Your Step-by-Step Guide
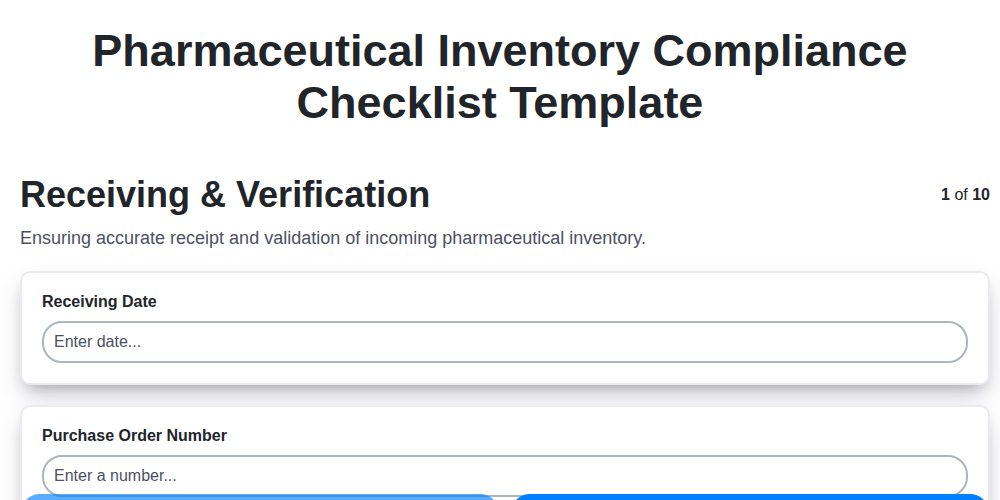
Mastering Medication Management: Your Pharmaceutical Inventory Compliance Checklist Template
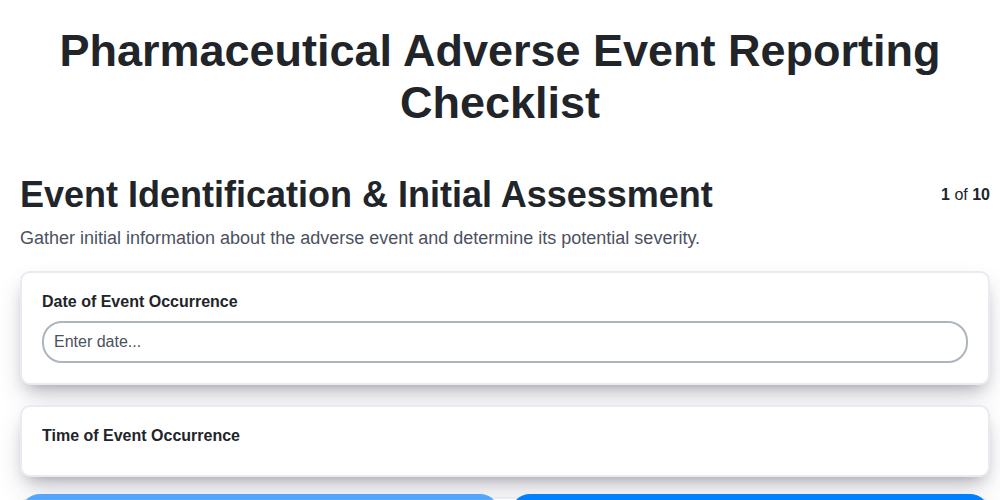
Navigating Adverse Event Reporting: Your Pharmaceutical Checklist Guide
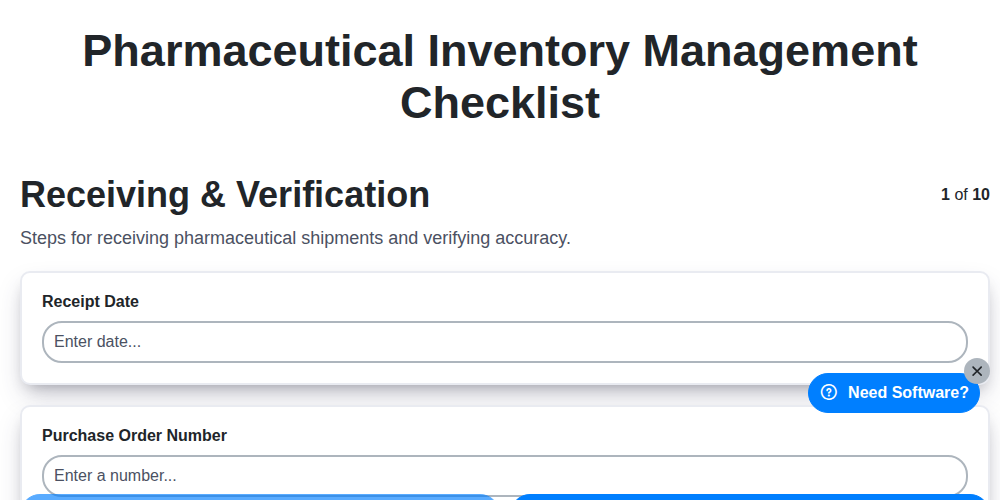
Pharmaceutical Inventory Management Checklist: Your Guide to Compliance & Accuracy
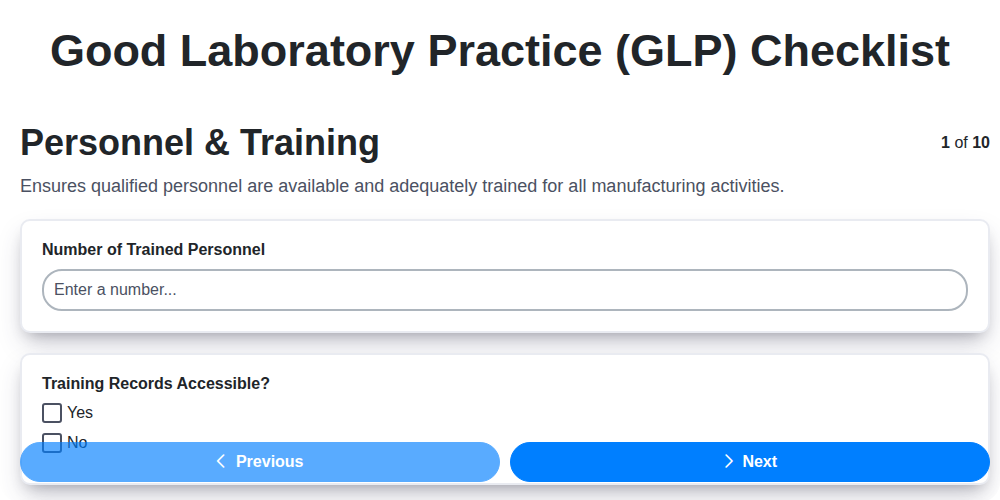
Your Essential GLP Checklist Template: A Practical Guide
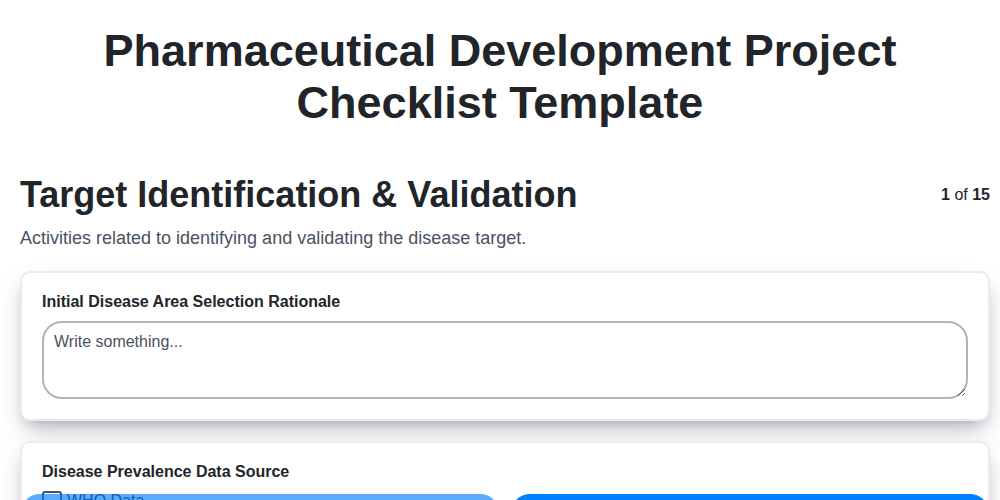
Your Pharmaceutical Development Checklist: A Template for Success
Pharmaceutical Validation Checklist Template: Your Guide to Compliance
We can do it Together
Need help with
Pharmaceutical?
Have a question? We're here to help. Please submit your inquiry, and we'll respond promptly.